Les cirrhotiques ont une hémodynamique particulière. Le noeud physiopathologique semble se jouer autour de l’hypertension portale (HTP). La fibrose hépatique modifie la vascularisation portale et un gradient porto-systémique apparait. L’HTP couplée à une augmentation de molécules vasodilatatrices induit une vasodilatation splanchnique. Ce secteur vasculaire va piéger une partie de la volémie créant une hypovolémie relative. Les mécanismes de compensation s’activent avec stimulation du système rénine-angiotensine et du système nerveux sympathique. La rétention hydro-sodée est importante mais la vasodilatation omniprésente piège « perpetuellement » ce volume. Le cercle vicieux se dessine avec la baisse des résistances vasculaires systémiques.
L’activation du système sympathique associé à une baisse des résistances vasculaires donnent un tableau hyperkinétique avec « l’impression que le ventricule gauche se bagarre pour générer une pression artérielle suffisante »
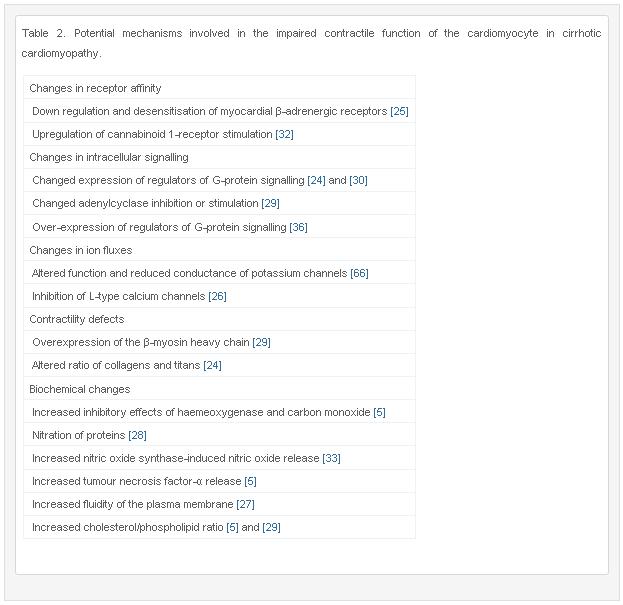
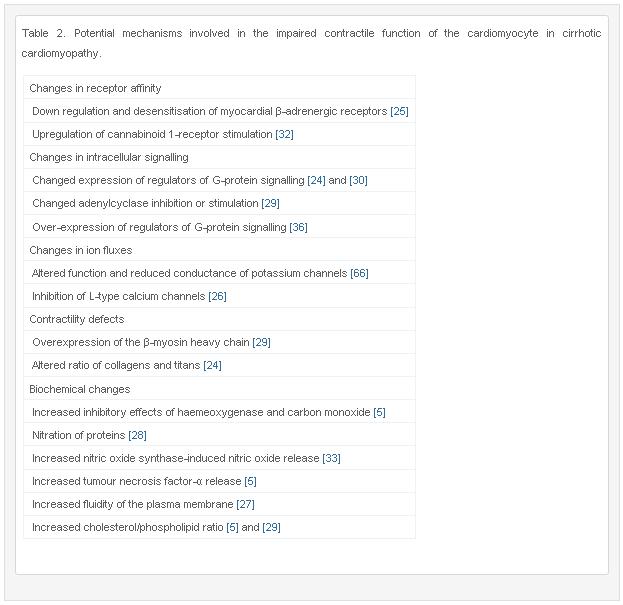
Chez le cirrhotique il y a de plus en plus de preuve de l’épuisement du coeur dans ce contexte hémodynamique particulier. Des anomalies systoliques, diastoliques et de la conduction cardiaque spécifique de la cirrhose (indépendamment de l’étiologie) sont possibles. La physiopathologie est complexe avec plusieurs pistes issues de modèles expérimentaux comme le résume ce tableau issu de l’article de Møller et al dans Int J Cardiolol
 Ce que je comprends de façon imagée, c’est que le coeur gauche perd en réserve contractile, s’épuise sur ce tableau hyperkinétique et qu’il devient peu efficace pour répondre à un effort ou un stress comme un sepsis. L’IRM cardiaque ou l’analyse du strain myocardique semblent être de bons outils pour dépister la dysfonction systolique du cirrhotique (ou l’échographie de stress ou d’effort).
Ce que je comprends de façon imagée, c’est que le coeur gauche perd en réserve contractile, s’épuise sur ce tableau hyperkinétique et qu’il devient peu efficace pour répondre à un effort ou un stress comme un sepsis. L’IRM cardiaque ou l’analyse du strain myocardique semblent être de bons outils pour dépister la dysfonction systolique du cirrhotique (ou l’échographie de stress ou d’effort).
Quant à la dysfonction diastolique, elle est liée à une rigidification de la paroi myocardique. Ce qui me frappe c’est que dans la littérature spécifique sur ce sujet on trouve la notion qu’un rapport E/A < 1 traduit de la gravité. C’est paradoxal par rapport à ce que j’avais retenu jusqu’alors de la dysfonction diastolique « en général ».
L’élongation du QT pourrait traduire une certaine forme de dysautonomie. De façon marquante il est très bien corrélé à l’HTP. Il semblerait qu’ils existent des anomalies du couplage électro-mécanique à cause d’une dysfonction de canaux potassiques et d’une agression par des cytokines pro-inflammatoires (sur bactériémies à bas bruit notamment)
Avant le D.U. d’échographie cardiaque, je ne connaissais pas toutes ces subtilités et je remercie les réanimateurs de la Croix-Rousse de m’avoir éclairé là dessus.
Ainsi la cardiomyopathie du cirrhotique est inquiétante lorsqu’elle est dépistée car elle signe l’équilibre précaire du cirrhotique avec un fort risque de syndrome hépato-rénal en cas de pertubation de l’équilibre instable. Tous ces éléments physiopathologiques aident à comprendre que la mise en place d’un TIPS peut être un vrai challenge hémodynamique pour ces patients et qu’il fallait insister sur l’évaluation cardiaque et la surveillance après la pose.
858234
NJXC3EEZ
1
vancouver
50
default
4213
https://www.nfkb0.com/wp-content/plugins/zotpress/
%7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22AJ26UTS4%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kazankov%20et%20al.%22%2C%22parsedDate%22%3A%222011%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EKazankov%20K%2C%20Holland-Fischer%20P%2C%20Andersen%20NH%2C%20Torp%20P%2C%20Sloth%20E%2C%20Aagaard%20NK%2C%20et%20al.%20Resting%20myocardial%20dysfunction%20in%20cirrhosis%20quantified%20by%20tissue%20Doppler%20imaging.%20Liver%20International%20%5BInternet%5D.%202011%20%5Bcited%202013%20Jun%2018%5D%3B31%284%29%3A534%26%23x2013%3B40.%20Available%20from%3A%20%3Ca%20class%3D%27zp-ItemURL%27%20href%3D%27http%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1111%5C%2Fj.1478-3231.2011.02468.x%5C%2Fabstract%27%3Ehttp%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1111%5C%2Fj.1478-3231.2011.02468.x%5C%2Fabstract%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Resting%20myocardial%20dysfunction%20in%20cirrhosis%20quantified%20by%20tissue%20Doppler%20imaging%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Konstantin%22%2C%22lastName%22%3A%22Kazankov%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Peter%22%2C%22lastName%22%3A%22Holland-Fischer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Niels%20H.%22%2C%22lastName%22%3A%22Andersen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Peter%22%2C%22lastName%22%3A%22Torp%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erik%22%2C%22lastName%22%3A%22Sloth%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Niels%20K.%22%2C%22lastName%22%3A%22Aagaard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hendrik%22%2C%22lastName%22%3A%22Vilstrup%22%7D%5D%2C%22abstractNote%22%3A%22Background%3A%20Cirrhotic%20cardiomyopathy%20is%20described%20as%20latent%20cardiac%20failure.%20However%2C%20it%20remains%20to%20be%20investigated%20whether%20the%20myocardial%20dysfunction%20is%20present%20even%20at%20rest.Aims%3A%20The%20aim%20of%20the%20present%20study%20was%20to%20quantify%20left%20ventricular%20function%20at%20rest%20by%20means%20of%20tissue%20Doppler%20imaging%20in%20patients%20with%20cirrhosis%20and%20relate%20the%20findings%20to%20liver%20status%20and%20cirrhosis%20aetiology.Methods%3A%20Forty-four%20consecutive%20patients%20and%2023%20age-matched%20healthy%20controls%20were%20included.%20Conventional%20echocardiographic-%20and%20tissue%20Doppler-derived%20indices%20of%20systolic%20and%20diastolic%20function%20were%20obtained.%20Liver%20function%20was%20quantified%20by%20the%20galactose%20elimination%20capacity%20and%20clinical%20stage%20by%20the%20Child%5Cu2013Pugh%20and%20MELD%20scores.Results%3A%20Both%20systolic%20and%20diastolic%20myocardial%20functions%20were%20compromised%20in%20the%20patients%20at%20rest.%20Left%20ventricular%20ejection%20fraction%20%2856.4%20%5Cu00b1%206.1%20vs.%2059.9%20%5Cu00b1%203.9%25%2C%20P%3C0.02%29%2C%20mean%20peak%20systolic%20tissue%20velocity%20%284.6%20%5Cu00b1%200.9%20vs.%205.6%20%5Cu00b1%200.7%20cm%5C%2Fs%2C%20P%3C0.001%29%20and%20mean%20systolic%20strain%20rate%20%28%5Cu22121.23%20%5Cu00b1%200.19%20vs.%20%5Cu22121.5%20%5Cu00b1%200.14%5C%2Fs%2C%20P%3C0.001%29%20were%20all%20reduced%20in%20cirrhosis%20patients.%20Thirty-four%20patients%20%2854%25%29%20had%20diastolic%20dysfunction%2C%2011%20had%20impaired%20diastolic%20relaxation%20pattern%20%2825%25%29%2C%2012%20had%20the%20more%20severe%20pseudonormal%20filling%20pattern%20%2827%25%29%20and%20one%20had%20restrictive%20filling%20or%20severe%20diastolic%20dysfunction%20%282%25%29.%20None%20of%20the%20echocardiographic%20findings%20were%20related%20to%20the%20cirrhosis%20aetiology.Conclusion%3A%20Tissue%20Doppler%20imaging%20during%20rest%20detected%20substantial%20systolic%20and%20diastolic%20myocardial%20dysfunction%20in%20cirrhotic%20patients.%20This%20supports%20the%20existence%20of%20a%20distinct%20cirrhotic%20cardiomyopathy.%22%2C%22date%22%3A%222011%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1478-3231.2011.02468.x%22%2C%22ISSN%22%3A%221478-3231%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1111%5C%2Fj.1478-3231.2011.02468.x%5C%2Fabstract%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T09%3A41%3A11Z%22%7D%7D%2C%7B%22key%22%3A%22NBS3RDEJ%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Krag%20et%20al.%22%2C%22parsedDate%22%3A%222010%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EKrag%20A%20a%2C%20Bendtsen%20F%2C%20Mortensen%20C%20a%2C%20Henriksen%20JH%2C%20Moller%20S.%20Effects%20of%20a%20single%20terlipressin%20administration%20on%20cardiac%20function%20and%20perfusion%20in%20cirrhosis.%20Journal%20of%20Gastroenterology%20%5BInternet%5D.%202010%20%5Bcited%202013%20Jun%2018%5D%3B22%289%29%3A1085%26%23x2013%3B92.%20Available%20from%3A%20%3Ca%20class%3D%27zp-ItemURL%27%20href%3D%27http%3A%5C%2F%5C%2Fovidsp.ovid.com%5C%2Fovidweb.cgi%3FT%3DJS%26CSC%3DY%26NEWS%3DN%26PAGE%3Dfulltext%26D%3Dovftl%26AN%3D00042737-201009000-00007%27%3Ehttp%3A%5C%2F%5C%2Fovidsp.ovid.com%5C%2Fovidweb.cgi%3FT%3DJS%26CSC%3DY%26NEWS%3DN%26PAGE%3Dfulltext%26D%3Dovftl%26AN%3D00042737-201009000-00007%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Effects%20of%20a%20single%20terlipressin%20administration%20on%20cardiac%20function%20and%20perfusion%20in%20cirrhosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Aleksander%20a%22%2C%22lastName%22%3A%22Krag%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Flemming%22%2C%22lastName%22%3A%22Bendtsen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christian%20a%22%2C%22lastName%22%3A%22Mortensen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jens%20H.%22%2C%22lastName%22%3A%22Henriksen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Soren%22%2C%22lastName%22%3A%22Moller%22%7D%5D%2C%22abstractNote%22%3A%22Background%3A%20The%20vasoconstrictor%20terlipressin%20is%20widely%20used%20in%20the%20treatment%20of%20the%20hepatorenal%20syndrome%20and%20variceal%20bleeding.%20However%2C%20terlipressin%20may%20compromise%20cardiac%20function%20and%20induce%20ischemia.%2C%20Aim%3A%20Therefore%2C%20we%20aimed%20to%20assess%20the%20effects%20of%20terlipressin%20on%20cardiac%20function%20and%20perfusion.%2C%20Methods%3A%20Twenty-four%20patients%20with%20cirrhosis%20and%20ascites%20participated%2C%20including%20nine%20with%20refractory%20ascites.%20Gated%20myocardial%20perfusion%20imaging%2C%20mean%20arterial%20blood%20pressure%20%28MAP%29%2C%20cardiac%20output%20%28CO%29%2C%20ejection%20fraction%20%28EF%29%2C%20end-diastolic%20volume%20%28EDV%29%2C%20perfusion%2C%20and%20motion%20of%20the%20myocardium%20were%20determined%20before%20and%20after%20a%20bolus%20injection%20of%202%20mg%20terlipressin.%2C%20Results%3A%20MAP%20increased%20after%20terlipressin%20%28P%20value%20of%20less%20than%200.001%29.%20EF%20and%20CO%20fell%20by%20-16%20and%20-17%25%2C%20respectively%20in%20the%20terlipressin%20group%20versus%201%20and%20-2%25%2C%20respectively%20in%20the%20placebo%20group%20%28P%20value%20of%20less%20than%200.001%20and%20P%20value%20of%20less%20than%200.01%29.%20In%20the%20terlipressin%20group%2C%20EDV%20increased%20by%2018%20versus%20-4%25%20in%20the%20placebo%20group%20%28P%20value%20of%20less%20than%200.01%29.%20Wall%20motion%20in%20the%20anterior%20and%20posterior%20walls%20fell%20by%20-18%20and%20-22%25%2C%20respectively%20after%20terlipressin%20treatment%20versus%200%20and%200%25%20in%20the%20placebo%20group%20%28P%20value%20of%20less%20than%200.01%29.%20In%20contrast%2C%20myocardial%20perfusion%20and%20stroke%20volume%20were%20unaltered%20in%20both%20the%20groups.%20The%20change%20in%20EF%20during%20terlipressin%20treatment%20correlated%20significantly%20with%20the%20change%20in%20MAP%20%28r%3D-0.60%2C%20P%20value%20%3C0.002%29.%20Patients%20with%20refractory%20ascites%20had%20a%20higher%20EF%20and%20lower%20EDV%20and%20ESV%20than%20the%20patients%20with%20nonrefractory%20ascites%2C%20both%20at%20baseline%20and%20after%20terlipressin%20treatment.%20The%20decrease%20in%20the%20left%20ventricular%20wall%20thickening%20and%20wall%20motion%20correlated%20with%20the%20Child--Pugh%20score%2C%20r%3D-0.59%2C%20P%3D0.005%20and%20r%3D-0.48%2C%20P%3D0.03.%2C%20Conclusion%3A%20In%20advanced%20cirrhosis%2C%20the%20increase%20in%20afterload%20and%20EDV%20after%20terlipressin%20treatment%20result%20in%20a%20decrease%20in%20left%20ventricular%20wall%20motion%2C%20resulting%20in%20reduced%20CO%20and%20EF%2C%20but%20myocardial%20perfusion%20is%20preserved.%20Alteration%20in%20cardiac%20function%20at%20baseline%20and%20after%20terlipressin%20treatment%20relates%20to%20the%20stage%20of%20decompensation.%2C%20%28C%29%202010%20Lippincott%20Williams%20%26%20Wilkins%2C%20Inc.%22%2C%22date%22%3A%222010%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1097%5C%2FMEG.0b013e32833a4822%22%2C%22ISSN%22%3A%220954-691X%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fovidsp.ovid.com%5C%2Fovidweb.cgi%3FT%3DJS%26CSC%3DY%26NEWS%3DN%26PAGE%3Dfulltext%26D%3Dovftl%26AN%3D00042737-201009000-00007%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T09%3A40%3A38Z%22%7D%7D%2C%7B%22key%22%3A%225XD5D4NI%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lee%20et%20al.%22%2C%22parsedDate%22%3A%221990%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3ELee%20SS%2C%20Marty%20J%2C%20Mantz%20J%2C%20Samain%20E%2C%20Braillon%20A%2C%20Lebrec%20D.%20Desensitization%20of%20myocardial%20%26%23x3B2%3B-adrenergic%20receptors%20in%20cirrhotic%20rats.%20Hepatology%20%5BInternet%5D.%201990%20%5Bcited%202013%20Jun%2018%5D%3B12%283%29%3A481%26%23x2013%3B5.%20Available%20from%3A%20%3Ca%20class%3D%27zp-ItemURL%27%20href%3D%27http%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1002%5C%2Fhep.1840120306%5C%2Fabstract%27%3Ehttp%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1002%5C%2Fhep.1840120306%5C%2Fabstract%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Desensitization%20of%20myocardial%20%5Cu03b2-adrenergic%20receptors%20in%20cirrhotic%20rats%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Samuel%20S.%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jean%22%2C%22lastName%22%3A%22Marty%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jean%22%2C%22lastName%22%3A%22Mantz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Emmanuel%22%2C%22lastName%22%3A%22Samain%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alain%22%2C%22lastName%22%3A%22Braillon%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Didier%22%2C%22lastName%22%3A%22Lebrec%22%7D%5D%2C%22abstractNote%22%3A%22Cardiac%20responses%20to%20catecholamines%20are%20known%20to%20be%20attenuated%20in%20chronic%20liver%20disease.%20To%20elucidate%20the%20role%20of%20%5Cu03b2-adrenergic%20receptor%20alteration%20in%20this%20phenomenon%2C%20we%20measured%20heart%20rate%20responsiveness%20to%20isoprenaline%20and%20myocardial%20%5Cu03b2-adrenergic%20receptor%5Cu2013binding%20characteristics%20in%20three%20groups%20of%20rats%3A%20those%20that%20were%20sham%20operated%2C%20those%20that%20had%20portal%20vein%20stenosis%20and%20those%20that%20were%20cirrhotic%20because%20of%20bile%20duct%20ligation.%20Responsiveness%20to%20isoprenaline%20was%20evaluated%20in%20conscious%20rats%20by%20the%20dose%20of%20isoprenaline%20needed%20to%20increase%20basal%20heart%20rate%20by%2050%20beats%5C%2Fmin%20and%20by%20the%20maximal%20heart%20rate%20response.%20%5Cu03b2-Receptor%20characteristics%20in%20heart%20membranes%20were%20derived%20from%20125I-iodocyanopindolol%20binding%20data.%20Compared%20with%20sham-operated%20controls%2C%20cirrhotic%20rats%20needed%20a%20significantly%20higher%20dose%20of%20isoprenaline%20to%20raise%20basal%20heart%20rate%20by%20%2850%20beats%5C%2Fmin%29.%20%28102.3%20%5Cu00b1%2019.1%20vs.%2028.3%20%5Cu00b1%2011.3%20ng%5C%2Fkg%29%20and%20lower%20maximal%20heart%20rate%20response%20%28104%20%5Cu00b1%2029%20vs.%20158%20%5Cu00b1%2061%20beats%5C%2Fmin%29.%20In%20addition%2C%20myocardial%20%5Cu03b2-receptor%20density%20was%20significantly%20lower%20in%20cirrhotic%20rats%20%2826.5%20%5Cu00b1%204.6%20vs.%2037.5%20%5Cu00b1%2010.3%20fmol%5C%2Fmg%20protein%29%20and%20the%20dissociation%20constant%20was%20higher%20%2831.6%20%5Cu00b1%2017.0%20vs.%2014.0%20%5Cu00b1%202.5%20pmol%5C%2FL%29.%20Analysis%20of%20%5Cu03b21%5C%2F%5Cu03b22%20subpopulations%20revealed%20that%20the%20decreased%20total%20%5Cu03b2-receptor%20density%20was%20entirely%20due%20to%20selective%20%5Cu03b21-receptor%20down-regulation.%20%5Cu03b2-Receptor%20affinity%20for%20agonist%20was%20not%20altered%20in%20cirrhotic%20rats.%20Rats%20with%20portal%20vein%20stenosis%20showed%20no%20significant%20differences%20in%20either%20isoprenaline%20responsiveness%20or%20%5Cu03b2-receptor%20characteristics%20when%20compared%20with%20controls.%20These%20results%20indicate%20that%20%5Cu03b2-adrenergic%20receptor%20down-regulation%20may%20be%20responsible%20for%20the%20myocardial%20hyporesponsiveness%20to%20catecholamines%20observed%20in%20cirrhosis.%20%28HEPATOLOGY%201990%3B12%3A481%5Cu2013485%29.%22%2C%22date%22%3A%221990%22%2C%22language%22%3A%22en%22%2C%22DOI%22%3A%2210.1002%5C%2Fhep.1840120306%22%2C%22ISSN%22%3A%221527-3350%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fonlinelibrary.wiley.com%5C%2Fdoi%5C%2F10.1002%5C%2Fhep.1840120306%5C%2Fabstract%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T07%3A45%3A30Z%22%7D%7D%2C%7B%22key%22%3A%22N5GPDWJE%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22M%5Cu00f8ller%20et%20al.%22%2C%22parsedDate%22%3A%222011-09%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EM%26%23xF8%3Bller%20S%2C%20Hobolth%20L%2C%20Winkler%20C%2C%20Bendtsen%20F%2C%20Christensen%20E.%20Determinants%20of%20the%20hyperdynamic%20circulation%20and%20central%20hypovolaemia%20in%20cirrhosis.%20Gut.%202011%20Sep%3B60%289%29%3A1254%26%23x2013%3B9.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Determinants%20of%20the%20hyperdynamic%20circulation%20and%20central%20hypovolaemia%20in%20cirrhosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S%5Cu00f8ren%22%2C%22lastName%22%3A%22M%5Cu00f8ller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lise%22%2C%22lastName%22%3A%22Hobolth%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christine%22%2C%22lastName%22%3A%22Winkler%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Flemming%22%2C%22lastName%22%3A%22Bendtsen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erik%22%2C%22lastName%22%3A%22Christensen%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Patients%20with%20advanced%20cirrhosis%20often%20develop%20a%20hyperdynamic%20circulation%20with%20central%20hypovolaemia.%20The%20events%20that%20initiate%20the%20systemic%20haemodynamic%20abnormalities%20and%20the%20coupling%20of%20these%20factors%20to%20splanchnic%20haemodynamics%20are%20still%20unclear.%20Objective%20On%20the%20basis%20of%20a%20large%20population%20of%20patients%20with%20cirrhosis%20to%20identify%20splanchnic%20and%20clinical%20characteristics%20associated%20with%20the%20development%20of%20the%20hyperdynamic%20circulation%20and%20survival.%5CnMETHODS%3A%20We%20included%20410%20patients%20with%20cirrhosis.%20In%20all%20patients%2C%20a%20full%20haemodynamic%20investigation%20was%20performed.%20The%20data%20were%20analysed%20using%20regression%20analyses%2C%20principal%20components%20analyses%2C%20and%20Cox%20proportional%20hazards%20analyses.%5CnRESULTS%3A%20Multivariate%20regression%20analyses%20showed%20that%20higher%20cardiac%20output%20was%20independently%20associated%20with%20higher%20hepatic%20venous%20pressure%20gradient%20%28HVPG%29%20and%20higher%20hepatic%20blood%20flow%20%28HBF%29%20%28p%3C0.00001%29.%20Higher%20heart%20rate%20was%20independently%20associated%20with%20presence%20of%20ascites%20and%20higher%20HVPG%20%28p%3C0.0001%29.%20Central%20blood%20volume%20and%20circulation%20time%20were%20independently%20associated%20with%20higher%20HBF%20and%20lower%20postsinusoidal%20resistance%2C%20respectively%20%28p%3C0.0001%29.%20Systemic%20vascular%20resistance%20was%20independently%20associated%20with%20lower%20HVPG%20%28p%3C0.0001%29.%20The%20final%20Cox%20proportional%20hazards%20model%20showed%20that%20decreased%20survival%20was%20independently%20associated%20with%20higher%20age%20%28p%3D0.003%29%2C%20lower%20blood%20haemoglobin%20concentration%20%28p%3D0.0006%29%2C%20higher%20plasma%20creatinine%20%28p%3D0.01%29%2C%20higher%20plasma%20alkaline%20phosphatase%20%28p%3D0.007%29%2C%20lower%20right%20atrial%20pressure%20%28p%3D0.004%29%2C%20and%20higher%20heart%20rate%20%28p%3D0.002%29.%5CnCONCLUSION%3A%20The%20development%20of%20the%20hyperdynamic%20circulation%20and%20central%20hypovolaemia%20are%20mainly%20explained%20by%20changes%20in%20portal%20pressure%20and%20HBF.%20Together%20with%20indicators%20of%20liver%20dysfunction%2C%20central%20hypovolaemia%20is%20associated%20with%20poorer%20prognosis.%22%2C%22date%22%3A%22Sep%202011%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1136%5C%2Fgut.2010.235473%22%2C%22ISSN%22%3A%221468-3288%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T07%3A43%3A50Z%22%7D%7D%2C%7B%22key%22%3A%22JCRSVGHD%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22R%5Cu00f6ssle%22%2C%22parsedDate%22%3A%222011-09%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3ER%26%23xF6%3Bssle%20M.%20Hyperdynamic%20circulation%20and%20portal%20hypertension%3A%20chicken%20or%20egg%3F%20Gut.%202011%20Sep%3B60%289%29%3A1167%26%23x2013%3B9.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hyperdynamic%20circulation%20and%20portal%20hypertension%3A%20chicken%20or%20egg%3F%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Martin%22%2C%22lastName%22%3A%22R%5Cu00f6ssle%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%22Sep%202011%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1136%5C%2Fgut.2011.242511%22%2C%22ISSN%22%3A%221468-3288%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T07%3A43%3A39Z%22%7D%7D%2C%7B%22key%22%3A%22W6MVI7BA%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22M%5Cu00f8ller%20and%20Henriksen%22%2C%22parsedDate%22%3A%222005%22%2C%22numChildren%22%3A1%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EM%26%23xF8%3Bller%20S%2C%20Henriksen%20JH.%20The%20systemic%20circulation%20in%20cirrhosis.%20Ascites%20and%20Renal%20Dysfunction%20in%20Liver%20Disease.%202005%3B139%26%23x2013%3B55.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20systemic%20circulation%20in%20cirrhosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22M%5Cu00f8ller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.H.%22%2C%22lastName%22%3A%22Henriksen%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222005%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22ISSN%22%3A%22%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T07%3A40%3A43Z%22%7D%7D%2C%7B%22key%22%3A%22FX2I6P7G%22%2C%22library%22%3A%7B%22id%22%3A858234%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22M%5Cu00f8ller%20et%20al.%22%2C%22numChildren%22%3A2%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EM%26%23xF8%3Bller%20S%2C%20Hove%20JD%2C%20Dixen%20U%2C%20Bendtsen%20F.%20New%20insights%20into%20cirrhotic%20cardiomyopathy.%20International%20Journal%20of%20Cardiology%20%5BInternet%5D.%20%5Bcited%202013%20Jun%2018%5D%3B%20Available%20from%3A%20%3Ca%20class%3D%27zp-ItemURL%27%20href%3D%27http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0167527312011953%27%3Ehttp%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0167527312011953%3C%5C%2Fa%3E%3C%5C%2Fdiv%3E%5Cn%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22New%20insights%20into%20cirrhotic%20cardiomyopathy%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S%5Cu00f8ren%22%2C%22lastName%22%3A%22M%5Cu00f8ller%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jens%20D.%22%2C%22lastName%22%3A%22Hove%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ulrik%22%2C%22lastName%22%3A%22Dixen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Flemming%22%2C%22lastName%22%3A%22Bendtsen%22%7D%5D%2C%22abstractNote%22%3A%22Cirrhotic%20cardiomyopathy%20designates%20a%20cardiac%20dysfunction%2C%20which%20includes%20reduced%20cardiac%20contractility%20with%20systolic%20and%20diastolic%20dysfunction%2C%20and%20presence%20of%20electrophysiological%20abnormalities%20in%20particular%20prolongation%20of%20the%20QT%20interval.%20Several%20pathophysiological%20mechanisms%20including%20reduced%20beta-receptor%20function%20seem%20involved%20in%20the%20autonomic%20and%20cardiac%20dysfunction.%20Cirrhotic%20cardiomyopathy%20can%20be%20revealed%20by%20tissue%20Doppler%20imaging%20but%20is%20best%20demasked%20by%20physical%20or%20pharmacological%20stress.%20Liver%20transplantation%20may%20revert%20cardiac%20dysfunction%20but%20surgery%20and%20shunt%20insertion%20may%20also%20aggravate%20the%20condition.%20Moreover%2C%20cirrhotic%20cardiomyopathy%20may%20contribute%20to%20heart%20failure%20after%20invasive%20procedures%20and%20to%20development%20of%20hepatic%20nephropathy%20as%20part%20of%20a%20cardiorenal%20syndrome.%20Whether%20beta-blockers%20have%20a%20deleterious%20effect%20in%20this%20clinical%20situation%20remains%20to%20be%20settled.%22%2C%22date%22%3A%22%22%2C%22language%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.ijcard.2012.09.089%22%2C%22ISSN%22%3A%220167-5273%22%2C%22url%22%3A%22http%3A%5C%2F%5C%2Fwww.sciencedirect.com%5C%2Fscience%5C%2Farticle%5C%2Fpii%5C%2FS0167527312011953%22%2C%22collections%22%3A%5B%22NJXC3EEZ%22%5D%2C%22dateModified%22%3A%222013-06-18T07%3A30%3A55Z%22%7D%7D%5D%7D
1.
Møller S, Hobolth L, Winkler C, Bendtsen F, Christensen E. Determinants of the hyperdynamic circulation and central hypovolaemia in cirrhosis. Gut. 2011 Sep;60(9):1254–9.
1.
Rössle M. Hyperdynamic circulation and portal hypertension: chicken or egg? Gut. 2011 Sep;60(9):1167–9.
1.
Møller S, Henriksen JH. The systemic circulation in cirrhosis. Ascites and Renal Dysfunction in Liver Disease. 2005;139–55.

^^ a bunch of PDF about this ^^
 Ce que je comprends de façon imagée, c’est que le coeur gauche perd en réserve contractile, s’épuise sur ce tableau hyperkinétique et qu’il devient peu efficace pour répondre à un effort ou un stress comme un sepsis. L’IRM cardiaque ou l’analyse du strain myocardique semblent être de bons outils pour dépister la dysfonction systolique du cirrhotique (ou l’échographie de stress ou d’effort).
Ce que je comprends de façon imagée, c’est que le coeur gauche perd en réserve contractile, s’épuise sur ce tableau hyperkinétique et qu’il devient peu efficace pour répondre à un effort ou un stress comme un sepsis. L’IRM cardiaque ou l’analyse du strain myocardique semblent être de bons outils pour dépister la dysfonction systolique du cirrhotique (ou l’échographie de stress ou d’effort).

4 réponses sur « La cardiomyopathie du cirrhotique »
Salut chef, et merci pour la biblio, sur un sujet aussi passionnant qu’obscure. Pour le flux mitral, le patient cirrhotique en hyperdébit à un flux mitral d’hyperdébit, c’est à dire une onde E très véloce, et une petit onde A. Le fait d’inverser ce rapport est éminemment suspect (si il existe par ailleurs un hyperdébit), car il traduit alors l’altération de la relaxation, au début sans élévation des pressions de remplissage. si la situation s’aggrave encore, les pressions de remplissages ne manqueront pas de s’élever, et il sera alors bien difficile d’interpréter un flux mitral à nouveau « pseudo-normal », de même que tous les indices habituelles de E/(quelque chose)…
Bref, je me comprends.
Merci encore, et à bientôt!
« Avant le D.U. d’échographie cardiaque, je ne connaissais pas toutes ces subtilités et je remercie les réanimateurs de la Croix-Rousse de m’avoir éclairé là dessus. »
Encore un qui a séché le cours anesthésie-réanimation du cirrhotique pendant son internat ;-))
PART
aie !
pris la main dans la sac !
J’aurais peut-être du écrire qu’avant le DU je n’étais pas mûr pour comprendre ou alors le cours a peut-être était décalé du fait de vacances improvisées :-p
ou alors le cours a peut-être était décalé du fait de vacances improvisées :-p
PS si t’as un cours en stock, je suis intéressé pour le lire
bye
Merci Rémi pour ce billet vraiment intéressant !!
En plus de la cardiopathie, le patient cirrhotique a comme tu l’as dit a une néovascularisation veineuse (dont la plus connue est les varices oesophagiennes). De ce fait, le volume veineux est augmenté, et en cas de veinodilatation (ex : anesthésie générale, sepsis), la précharge baisse proportionnellement à ce volume veineux. On sait tous que le patient cirrhotique est plus à risque de se « casser la gueule à l’induction ».
Amicalement
Minh